While menopause is generally seen as something every woman goes through, some will find it turns up much earlier than expected. For those who go through premature menopause, hot flashes, sleepless nights, and unpredictable periods can appear alongside the other challenges of being in your 20s or 30s.
Discover your personalized treatment options
At what age can menopause start?
Menopause happens when your ovaries stop releasing an egg each month and periods cease. Menopause is defined as 12 months since your last period. Find out more about the stages of menopause.
The average age for menopause in developed countries is between 50 and 52, and slightly lower in the developing world. This is an average, meaning that some will go through menopause later, and others earlier. Generally, the decade between ages 45 and 55 is the prime time for menopausal symptoms.
For a small number of people, things don’t go quite according to plan and menopause can happen years or even decades earlier.
How common are premature and early menopause?
You can go through menopause at any age after first getting your period, although the younger you are the less common this becomes.
- Around 1 in 20 will naturally go through menopause by age 45. This is known as early menopause
- A smaller number – around 1 in 100 – will have gone through menopause by age 40. This is premature menopause, also known as premature ovarian insufficiency (POI)
- It is estimated that 1 in 1000 will go through menopause before age 30
For simplicity, in this article, we will use the term early menopause to include all of these conditions unless otherwise specified.
Why does early and premature menopause happen?
For most who go through early menopause, there is no clear cause or certain medical conditions and procedures can be responsible.
Causes of early menopause
Latrogentic (medical) menopause
Some medical treatments can make early menopause more likely:
- Chemotherapy. In the same way that chemotherapy agents damage and kill off cancerous cells, they can also damage the ovaries. In some cases, this may lead to early menopause
- Radiotherapy.Especially when applied to the abdomen or pelvis, radiotherapy can have similar effects as chemotherapy. If you are going through cancer treatment, your oncologist will be able to explain the possible side effects, including implications for your ovarian function and fertility
- Some types of surgery. Perhaps the most obvious is where the ovaries are removed surgically, a procedure known as oophorectomy. This can be done to remove cysts, tumors, and, decrease the risk of recurring pain with endometriosis as well as to reduce the risk of ovarian cancer if you are a carrier of a BRCA or other gene mutation that increases your risk of ovarian cancer. If you have had this type of surgery, your healthcare provider will discuss menopause and HT around the time of your procedure. Other forms of surgery can also have an impact on your age at menopause. One study of women aged 46 and under found that removal of the uterus (hysterectomy) while leaving the ovaries in place was associated with going through menopause an average of 3.7 years earlier. Similar effects have been observed in those who have had surgery for endometriosis, and in those who have had ovarian drilling for PCOS (polycystic ovary syndrome)
Read more about surgical or induced menopause.
Autoimmune conditions
Around 1 in 20 cases of early or premature menopause are related to autoimmune conditions including type 1 diabetes, Addison’s disease, some types of arthritis, and thyroid conditions among others. This is because the body’s immune system mistakenly attacks its own organs and tissues.
In some cases, primary ovarian insufficiency (POI), also known as premature ovarian failure, is considered an autoimmune condition in its own right, especially when it forms part of one of the so-called polyglandular autoimmune syndromes. These are rare genetic syndromes that cause clusters of autoimmune illnesses.
While having an autoimmune condition does not necessarily mean you will go through menopause early, talk to your healthcare provider if you notice menopause symptoms.
Likewise, POI can be the first of a cluster of autoimmune conditions to present itself. If you have been through menopause before the age of 40 and think you may be suffering from another autoimmune condition, talk to your healthcare provider.
Genetics
Many different genetic causes of early and premature menopause have been identified. The most common of these is Turner syndrome, in which the affected person has only one X chromosome rather than the usual two.
It’s thought that 50% of those who go through menopause before the age of 20 is due to a genetic cause.
Is early menopause different from spontaneous menopause in any way?
Early and premature menopause can be slightly different from menopause which occurs at a more usual time. With early menopause, hormone levels tend to be more unstable, and even after diagnosis, some may go through periods of relatively normal ovarian function, including having normal menstrual periods and even getting pregnant.
Those who go through early menopause as a result of medical or surgical treatment tend to have more severe and longer-lasting symptoms than those who go through spontaneous menopause. This is thought to be due to the sudden decrease in hormone levels (as opposed to the slow decline seen in natural menopause).
Early menopause symptoms
Menopause symptoms can vary widely but are the same no matter what age you go through menopause. They often include:
- Irregular or absent periods, or change to bleeding pattern
- Hot flashes
- Night sweats
- Poor sleep
- Weight gain
- Hair loss
- Mood changes
- Brain fog or difficulty concentrating
- Vaginal changes (especially dryness, burning and painful sex)
These can also be signs of other conditions, particularly in younger people. It is therefore sensible to check in with your healthcare provider for a full evaluation.
Find out more about the 34 most common menopause symptoms or take a look in our menopause symptoms library.
Is there an early menopause test?
Depending on your symptoms, your healthcare provider may perform a physical exam, including a pelvic exam and order blood tests to see if you are experiencing early menopause. These can include blood tests for the hormones FSH (follicle-stimulating hormone) and LH (luteinizing hormone) among others.
If these suggest menopause, they will usually be repeated after 4-6 weeks to confirm the result and to ensure that it is not simply the result of a normal hormonal fluctuation.
Should you talk to your healthcare provider?
See your healthcare provider if you have any symptoms of menopause, or if you are concerned about the possibility of early menopause for any other reason, including previous cancer treatment or family history.
Your healthcare provider will find it useful to have a record of your recent periods, which you may keep either on paper or on an app like Clue, Flo or Ovia Fertility.
They may also ask about any medications you use, any family history of early or premature menopause, and any other medical conditions which may be related.
Discover your personalized treatment options
How is early menopause treated?
HT
Those with premature menopause may be able to be treated with hormone therapy (HT) depending on their medical history and lifestyle. Your healthcare provider will be able to help you decide on the best type of HT to suit your lifestyle and needs. When it comes to HT, there is no one-size-fits-all solution and you may need to try a few different types before finding the best treatment for you.
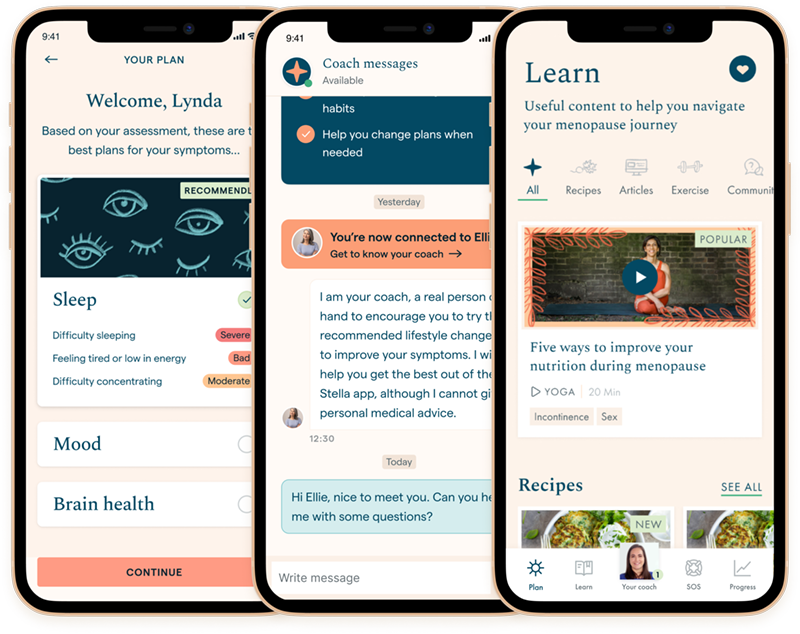
If you have gone through early menopause due to surgical treatment, you may need higher doses of estrogen to control your symptoms. The best way to work out whether your HT is adequate is to keep a log of your symptoms. You can do this either on paper or using an app, such as Stella, and share this information with your healthcare provider who will be able to adjust your dose as needed.
Combined contraceptive pill
The combined oral contraceptive pillis an alternative to HT for some people. This is especially useful if you are still at risk of pregnancy and would also like a reliable contraceptive. Again, your healthcare provider will be able to advise if this is an appropriate choice for you.
Lifestyle changes
These may also help with your symptoms. Common recommendations include maintaining a healthy diet, getting regular exercise, and cutting down on alcohol and caffeine.
What about your fertility?
If you have gone through menopause due to the removal of the ovaries or uterus, you will be unable to get pregnant. Your specialist will be able to discuss the implications of this and any alternatives to surgical treatment before the procedure.
If you go through spontaneous premature menopause, you may still become pregnant. This is because hormone levels and ovarian health are variable in this condition between 5% and 10% of those with POI become pregnant after diagnosis. This means that it is still important to use appropriate contraception if needed.
Read more about menopause contraception.
If fertility is a worry for you, it’s important to seek help early on if you are hoping to have a baby. Although it is still theoretically possible to get pregnant, it is much more difficult if you have been diagnosed with early menopause. This is because your menstrual cycle is likely to be irregular, and your ovaries will be releasing eggs much less frequently that may not be able to be fertilized.
If you have already been through menopause, it is generally thought that freezing eggs or embryos is less likely to be successful. It is, however, important that you are assessed properly by a fertility specialist as your options depend on several factors and can vary widely from person to person.
If you have not yet been through menopause but are at risk of POI – for example, if you are facing cancer treatment or have a strong family history of premature menopause – it may be worth discussing your options with a fertility specialist. This may include freezing eggs or embryos.
How does early menopause impact your long-term health?
While menopause is a normal part of life, early menopause comes with a few extra health considerations.
Mental health
Taking care of your mental health is especially important. While we know that hormonal changes can increase your risk of anxiety and depression, early menopause can be particularly difficult to deal with for other reasons too.
You may find yourself coping not only with the physical aspects of menopause but also fertility issues and the social implications of going through menopause at a much earlier age than expected. Who wouldn’t find this difficult? You don’t need to feel alone and your healthcare provider will be able to advise on treatment options including medications and talking therapies.
You don’t need to feel alone and your doctor will be able to advise on treatment options including medications and talking therapies.”
Cardiovascular disease
There are physical health issues to take into consideration too. After menopause, you are at greater risk of cardiovascular disease (including heart disease, stroke, and blood clots) due to hormonal changes. Some studies have suggested that this risk is increased further in those who go through menopause early. One large cohort study of over 140,000 women found that natural premature menopause increased the risk of cardiovascular disease by 36%. This figure was even higher in those who went through premature menopause due to surgery, with an 87% increased risk.
Although there has been fierce debate and mixed evidence about the role of hormone therapy (HT) in preventing cardiovascular disease, current thinking is that it may help to reduce your risk. This is one of the reasons that HT should usually be prescribed in cases of premature menopause.
It is also sensible to pay attention to your wider cardiovascular health if you go through premature menopause. Your healthcare provider will be able to advise on how to approach your own personal risk factors, which may include smoking, having high blood pressure or high cholesterol, and being overweight or obese.
Bone health
Premature menopause in particular has been linked with thinning of the bones (osteoporosis and osteopenia) and subsequent increased risk of fractures. If you are diagnosed with POI, your healthcare provider will discuss bone density testing, as well as using HT to help slow or prevent this process. It is also important to have a balanced diet with plenty of calcium and vitamin D, and to get plenty of weight-bearing exercises to strengthen the bones.
Cognitive impairment
Surgery to remove the ovaries before the usual age of menopause has been linked to an increased risk of cognitive impairment, dementia, and Parkinson’s disease in later life.
This surgery has also been linked with an increased risk of two conditions that affect the eye: macular degeneration and glaucoma. If you are concerned about symptoms of any of these conditions, see a healthcare provider. It is thought that HT may have a beneficial effect on this.
Sexual health
Finally, don’t forget contraception! Ovarian function can suddenly return even if you have not had periods for many years. Your healthcare provider will be able to help you choose the right contraceptive for you. Bear in mind that although HT contains the same hormones as many contraceptives, it will not prevent pregnancy.
Condoms are also important to protect you from sexually transmitted infections.
Can you prevent early menopause?
If you smoke, it is worth making a real effort to stop as soon as possible. Smokers have been found to go through menopause on average just under two years earlier than non-smokers.
Otherwise, there is not a great deal that you can do to prevent or delay menopause, although we would always recommend following a healthy diet and lifestyle.
Read more about menopause on our blog or in our symptoms library.