What kind of headaches could you experience?
Many different kinds of headaches can affect you at the time of menopause. The two most common are:
1. Migraines. These are usually one-sided headaches that may be associated with nausea, vomiting, and sensitivity to light and noise. Migraines can be preceded by sensory changes known as aura. Auras often cause changes to your vision, including seeing flashing lights or zigzag lines. Migraines can be severe and can last for hours
2. Tension headaches. They are often described as a band-like pain or pressure around the head which lasts from 30 minutes to several hours
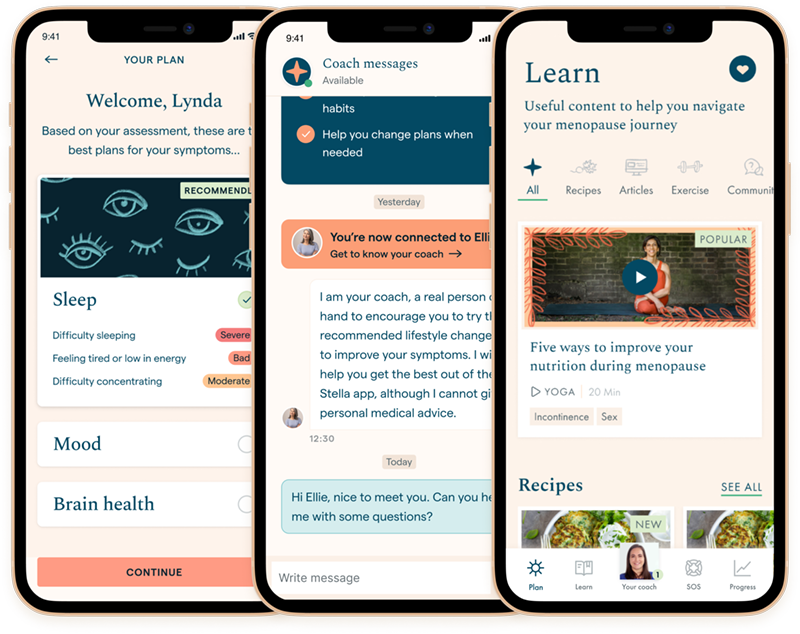
Discover your personalized treatment options
What do menopause headaches feel like?
Maybe you don’t realize what you are feeling is a headache, just that you have noticed strange head sensations in menopause. Headaches can present in a variety of ways. Here are a few symptoms of headaches:
- Strange head sensations
- Pulsing in your head
- Throbbing sensation
- The feeling of a tight band around your head
- Buzzing feeling
- Sensitivity to light or sound
- Nausea
- Fatigue
- Dizziness
Menopause headaches can affect other symptoms, including sleep issues, anxiety and depression.
How likely are headaches at menopause?
- Fairly common
- One study of over 500 postmenopausal women found that 13.7% of them suffered from headaches
- Of these, 82% said that their headaches had started prior to menopause
Read more about the stages of menopause or aches and pains symptoms.
How can you reduce perimenopause headaches?
1. Diary. Try keeping a diary of your headaches, including dates, times, symptoms, and possible triggers. This will help you and your healthcare provider to identify any patterns, especially if your headaches are linked to your menstrual cycle.
2. Healthy lifestyle. Minimize alcohol, caffeine, and any other known headache triggers. Do exercise that increases your heart rate and try to get enough sleep by establishing a routine.
3. Talk to your healthcare provider. Headaches can be caused by several different conditions, many of which can be treated effectively once they are diagnosed.
4. Relax. Create calm with relaxing activities, such as yoga and acupuncture.
Can hormone therapy (HT) help?
HT is not a treatment for migraines, although those with migraines can use certain types of HT to control other menopausal symptoms. People with headaches have a variable response to HT. Overall, migraines generally get worse with hormone treatment.
If you are taking HT to control other menopausal symptoms and find that it makes your headaches worse, you may benefit from switching to a transdermal preparation (HT patch or gel), or from a reduced dose of estrogen.
For those with migraines, a transdermal preparation (HT patch or gel) is usually the safest. This is because those who regularly experience migraines may be at risk of certain conditions, such as a stroke. Taking the HT transdermally greatly reduces this risk.
Although HT is beneficial for some, it is not suitable for everyone. Speak to your healthcare provider about whether it is right for you.
Read more about HT risks and benefits.
Headaches and menopause FAQs
Keeping a diary has helped me figure out that too much caffeine triggers my headaches.