VAGINAL PROLAPSE DEFINITION
Vaginal prolapse happens when the muscles and connective tissue that support the organs in your pelvis weaken.
This weakening means your uterus, urethra, bladder, or rectum become more likely to drop down into your vagina. If your pelvic floor muscles weaken enough, one or more of these organs can even bulge out of your vagina.
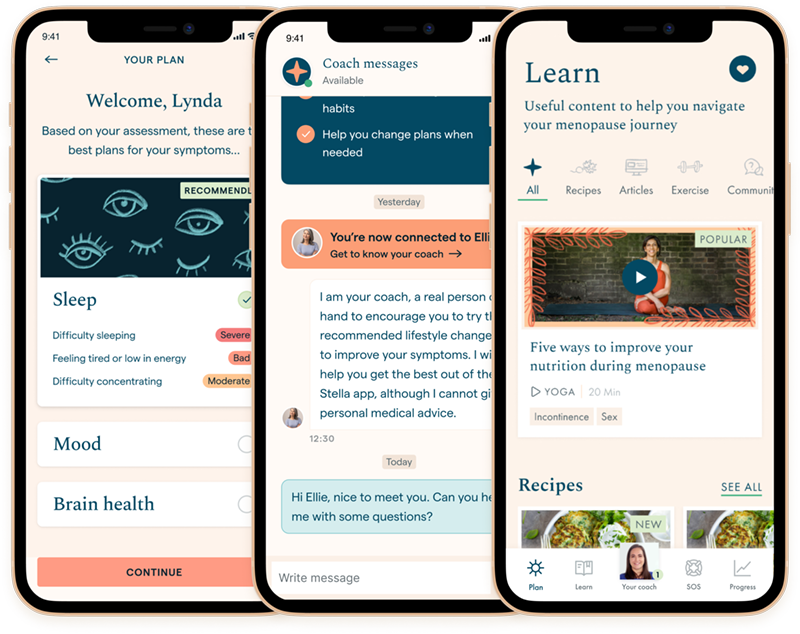
Discover your personalized treatment options
FOUR TYPES OF VAGINAL PROLAPSE
- Anterior prolapse – Your bladder bulges into the front wall of your vagina
- Uterine prolapse – Your uterus bulges into your vagina
- Vaginal vault prolapse – The top of your vagina sags down after your uterus has been removed
- Posterior wall prolapse – Your rectum bulges into the back wall of your vagina

HOW LIKELY IS MENOPAUSE PROLAPSE?
- While vaginal prolapse can happen at any time during your life, it is most commonly diagnosed during the later stages of postmenopause
- You are more at risk to have some form of prolapse during menopause and postmenopause if you had a full-term pregnancy. You also have more risk if you have had one or more vaginal deliveries compared to only C-sections
- This likelihood increases for those who have had more extensive tears during delivery and required forceps or vacuum delivery
Read more about the stages of menopause.
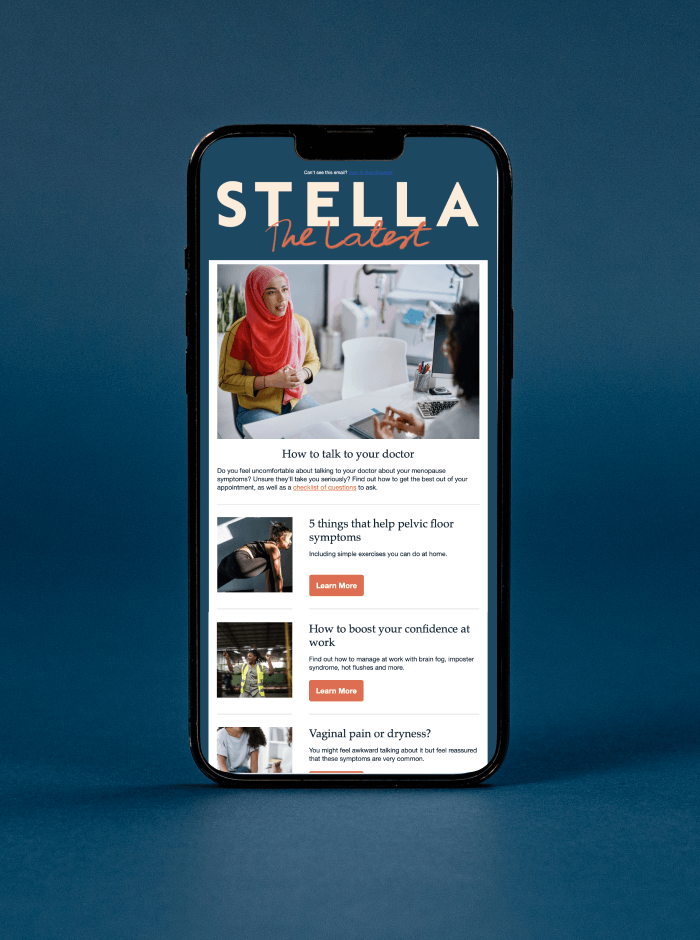
Sometimes, menopause prolapse has no symptoms and is found during an internal examination carried out for another reason, such as cervical screening. You may have other symptoms, such as vaginal discomfort, urinary incontinence or urinary tract infections (UTIs).
VAGINAL PROLAPSE TREATMENT
The first thing to do is talk to your healthcare provider about your symptoms as a pelvic examination is usually required to properly diagnose prolapse. They may recommend:
Pelvic floor exercises
You can do them anywhere and they are effective in strengthening your pelvic floor. It’s never too early to start doing them! The most important thing is accuracy – learning how to do the exercises properly – and consistency, remembering to do them every day.
Estrogen
If your prolapse is mild it may be recommended that you take estrogen in the form of a cream, or tablet you insert into your vagina or a vaginal ring. A pessary is a silicone ring that comes in several shapes and sizes and supports your vaginal walls and pelvic organs. It is fitted by a specialist nurse or gynecologist.
Surgery
If the symptoms from your prolapse continue to be bothersome even after initial treatments, your healthcare provider may refer you to a urogynecologist – a healthcare provider who specializes in problems like prolapse, incontinence, and bladder pain. They may talk to you about:
- Surgical repair to lift and support your pelvic organs
- Hysterectomy if you have a prolapsed uterus and you do not want any more kids
Vaginal prolapse and menopause FAQs
I need to know if sex is part of my future