Urinary incontinence definition
Urinary incontinence (UI) is the medical name for loss of bladder control or involuntary urine leakage. It means that you pee unintentionally – how and when this happens depends on what type of urinary incontinence you have.
Stress incontinence. Pee leaks when your bladder is under pressure, such as when you cough, laugh, exercise, or lift something heavy. You might experience a small leak or complete loss of control.
Urge/urgency incontinence. Also known as an overactive bladder, this is when pee leaks when you feel a sudden, often intense urge to pee. You may also feel a constant urge to pee, even when your bladder is empty.
Even if you don’t actually leak, and just feel the constant need to pee, an overactive bladder can be uncomfortable and disruptive to your life. Nighttime leakage, and being woken up by your bladder are also common symptoms.
Overflow incontinence. It may seem a bit unexpected, but difficulty emptying your bladder completely can also lead to stress incontinence and an overactive bladder. This is called overflow incontinence.
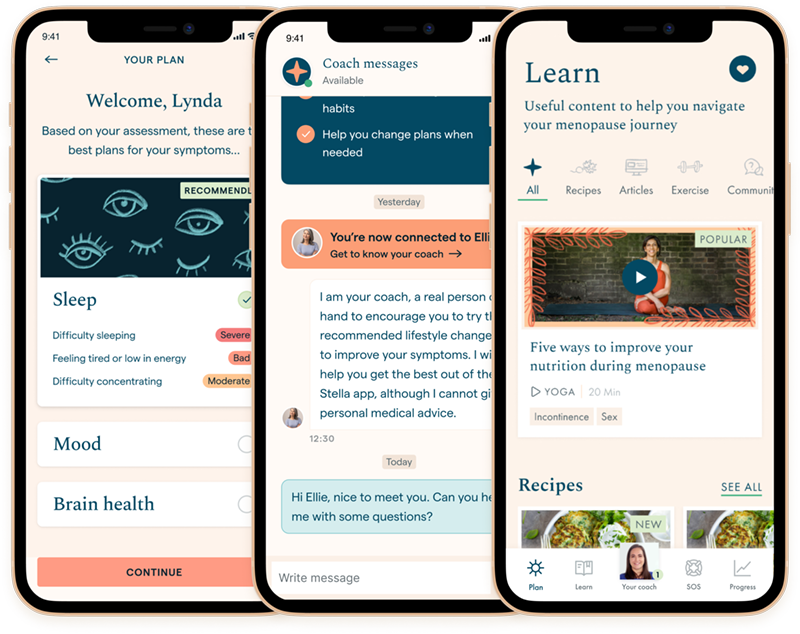
Discover your personalized treatment options
How likely is menopause incontinence?
- It affects 30 – 40% during perimenopause, rising to 50% postmenopause
- Those who have been pregnant, particularly those that have had vaginal deliveries, are more likely to suffer from this than those who have not
- Your weight, alcohol, nicotine, and caffeine consumption, and being on certain medications can also increase the risk of urinary incontinence
- Having a urinary tract infection can also cause temporary urinary incontinence
Read more about the stages of menopause.
How to cope with incontinence in menopause
You may experience other menopause symptoms alongside incontinence, including vaginal prolapse or anxiety. Here are some short-term fixes:
1 Know where the bathroom is. If you are going out, make sure you know in advance where the nearest toilets are. Always make sure you have some change for the bathroom handy. Consider carrying a change of underwear with you in a resealable plastic bag, to store the wet one.
2 Research incontinence pads. You can buy from a supermarket super absorbent pads and underwear to manage leaks or to help you when exercising. This kind of underwear has improved hugely in terms of style and function – you can find plenty of companies online that make attractive absorbent underwear.
3. Protect your bed. Online you can buy mattress protectors and washable or disposable absorbent sheets. There are also hand-held urinals and bedside commodes available. You can also speak to your healthcare provider about devices that can be placed into the vagina or urethra to prevent urine leakage.
These fixes aren’t sustainable long-term and we recommend talking to your healthcare provider.
Treatment for bladder weakness in menopause
Strengthen your pelvic floor
Doing daily pelvic floor exercises can help improve menopause bladder leakage.
Train your bladder
Plan your trips to the bathroom during the day to gradually increase the amount your bladder can hold.
Adjust your lifestyle
Limit caffeine and alcohol as they are diuretics, making you pee more. Drink the recommended amount of water and not too much.
Losing weight reduces the pressure on your bladder and pelvic floor region.
Talk to your healthcare provider about medication
Some suffer so much from urgency, going to the toilet many times, and are uncomfortable with the feeling of always needing to pee. Thankfully some medications can help and provide some relief while doing pelvic floor strengthening.
Surgical procedures for urge incontinence
Your healthcare provider may refer you to a urogynecologist to discuss possible surgical options.
Botulinum Toxin A injections
Botox is injected into the walls (muscle) of your bladder, and acts to partially paralyze the muscle so it is less overactive. The effects can last several months and you can have repeat injections if needed
Sacral nerve stimulation / posterior tibial nerve stimulation
The bladder muscle is controlled by passing an electrical current through the nerves that control the bladder
If you still suffer terribly from urge incontinence and the above treatments have not worked, there are some other procedures available.
Surgical procedures for stress incontinence
For stress incontinence, the main treatment is activating and strengthening your pelvic floor. Typically you would do this with a pelvic floor physical therapist. If you are still suffering, you may be referred to a urogynecologist to discuss surgical procedures which may help.
Sling surgery
A sling is placed around the neck of your bladder to support it. This outpatient procedure has a high success rate in women with moderate to severe incontinence.
Urethral bulking agents
This is injected into your urethra’s walls to allow the urethra to close with more force.
Incontinence and menopause FAQs
The fear of going somewhere new where you do not know where the bathrooms are can be overwhelming